Shoulder Pain
Shoulder Pain
There has recently been a high amount of attention drawn to the efficacy of common treatments for shoulder pain within the media, health care professionals and the scientific literature. In this month’s newsletter, Musculoskeletal Physiotherapist Mike Callan will dive into sub-acromial decompression (SAD) surgery and cortisone injections, summarising the latest evidence. He will also look at evidence based conservative management for shoulder pain.
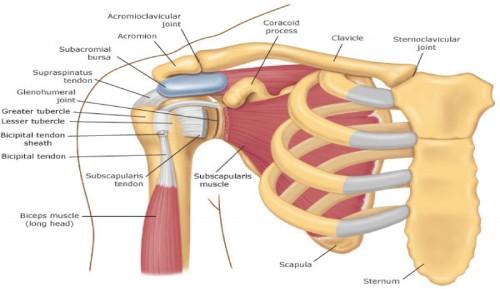
Shoulder pain is common and can be very complex. There are many structures around the shoulder that can be sources of pain, and many of these blend together. For our purposes, we will be talking about sub-acromial pain. Sub-acromial pain originates from any of the tissues that are inside the shoulder, such as the tendons of the rotator cuff and biceps muscle, shoulder joint, or the various ligaments and bursae.
In the 1970s, the common thought for why shoulder pain developed was ‘impingement’. The idea was that repeated ‘pinching’ of the rotator cuff tendons and bursa against the roof of the shoulder (acromion) when the arm was lifted overhead caused shoulder pain, injury to the tendons of the rotator cuff, and bursitis. If continued, this would lead to bone spurs, which in turn would rub against the rotator cuff and cause tears. This was also thought to be associated with the shape of the acromion, as a more hooked shape acromion would cause more of this pinching.
As a result, acromioplasty, also known as subacromial decompression surgery was developed. The idea was to surgically remove the proposed source of irritation by shaving away bone spurs. This would create more space and decrease pinching in the shoulder, leading to both short-term and long-term pain relief, including risk of rotator cuff tearing. This has led to an incredible increase in SAD surgeries.
Numerous studies and reviews of the evidence have shown this to be highly questionable. Many symptoms of shoulder pain are associated with overload or underload of rotator cuff tendons and failure of these tendons, combined with lifestyle, genetics, hormones and age(1, 2). Also, a majority of tears in the rotator cuff happen on the underside, not the top where supposed bone spurs would affect the tendon. Additionally, the incidence of rotator cuff tears in people without shoulder pain is relatively common, with one study showing 52%(4) and another showing 50% in those over 70(4).
Despite the high cost of SAD surgeries, studies have shown that there is no difference in outcome between surgery and a graduated exercise program both one and two years after surgery(1,2). Eighty percent of those on waiting lists for surgery who underwent a 12-week rehabilitation program improved and chose not to undergo surgery(1). The results of the recent Can Shoulder Arthroscopy Work trial showed that SAD surgery was not more effective than sham surgery (placebo), which puts strong doubt on the efficacy of this surgery(2). This trend also carries over to those with rotator cuff tears. A study has shown no difference between physiotherapy exercise program, physiotherapy and SAD surgery, or physiotherapy and SAD and rotator cuff repair at a one year follow-up for those with non-traumatic partial rotator cuff tears(1,2). For those with full thickness rotator cuff tears, non-operative management consisting of graduated exercise was effective at 2-year follow-up, reducing the need for surgery by 75%(3). It has been proposed that the prolonged rest following surgery, followed by the gradual strengthening and increased loading around the shoulder is what is responsible for increased function, not the actual surgery itself(1,2).
Another highly used intervention for shoulder pain is corticosteroid injections. The commonly held idea is that repeated impingement in the shoulder causes inflammation in the subacromial bursa, which leads to pain. Although this is common practice, there is a lack of evidence for the efficacy of steroid injections for shoulder pain(1). Additionally, there is evidence to suggest that steroids can have a negative effect on rotator cuff tendons long term1.
So if you have shoulder pain, but the evidence for high cost interventions are lacking, what should you do? Currently, the evidence suggests gradual conditioning and loading of the muscles around the shoulder, mainly the rotator cuff and scapular muscles, as well as increased general physical activity(1,2). Managing overall workloads, particularly avoiding prolonged inactivity followed by periods of high demand, commonly called booming and busting, and adopting a pattern of regular use of the shoulder with gradual increase in load or difficulty is recommended. Also, addressing any big picture lifestyle factors that might increase pain sensitivity in the body, like lack of sleep, high stress, or high fear of re-injury are also recommended. As each person is different, individualised care is indicated. An experienced Physiotherapist can, after thoroughly assessing a shoulder problem, highlight which of these factors are driving the shoulder pain and come up with an individualised management plan to assist recovery.
References
1. Bloodletting for pneumonia, prolonged bed rest for low back pain, is subacromial decompression another clinical issusion? Lewis, J. Br J Sports Med 2015; 49:280-281
2. The End of an Era? Lewis, J. J Orthop Sports Phys Ther 2018; 48(3): 127-129.
3. What happens to patients when we do not repair their cuff tears? Five-year rotator cuff quality-of-life index outcomes following nonoperative treatment of patients with full-thickness rotator cuff tears. Boorman RS et al. J Shoulder Elbow Surg 2018 Mar; 27 (3): 444-448.
4. Rotator Cuff Tendinopathy: Navigating the Diagnosis-Management Conundrum. Lewis, J,et al. J Orthop Sports Phys Ther 2015 Nov; 45 (11): 923-936.
Author

Mike Callan
Senior Musculoskeletal Physiotherapist
Curtin University 2010
Mike Callan is a Musculoskeletal Physiotherapist. He has interest in managementof all musculoskeletal disorders, including shoulder pain and low back pain. He recently attended the NOI group Pain Adelaide conference, where he enjoyed learning new research and expert opinion on pain management.
Location
Opening Hours
Monday-Friday 7am-7pm
Saturday 8am-12pm