Is Your Pelvis Out Of Line?
Is your pelvis out of alignment? Facts about the pelvic joints
This month’s newsletter is by our Senior Musculoskeletal Physiotherapist Rob Waller. Rob has a special interest in spinal pain and has been author on multiple peer-reviewed publications on spinal pain. He also teaches at Curtin University, including in how to manage spinal pain, and is currently completing a PhD investigating pain mechanisms in young adults of the Raine Study (http://www.rainestudy.org.au).
As Physiotherapists we routinely assess and manage low back pain and pelvic girdle pain (PGP). The most common source of PGP symptoms is the sacroiliac joint (SIJ). More than 70% of women experience lumbopelvic pain during pregnancy, with most PGP resolving within three months post-pregnancy and up to 10% still experiencing pain and disability at two years. Other presentations of PGP are associated with trauma such as a car accident or a fall onto the buttock, and inflammatory conditions such as ankylosing spondylitis.
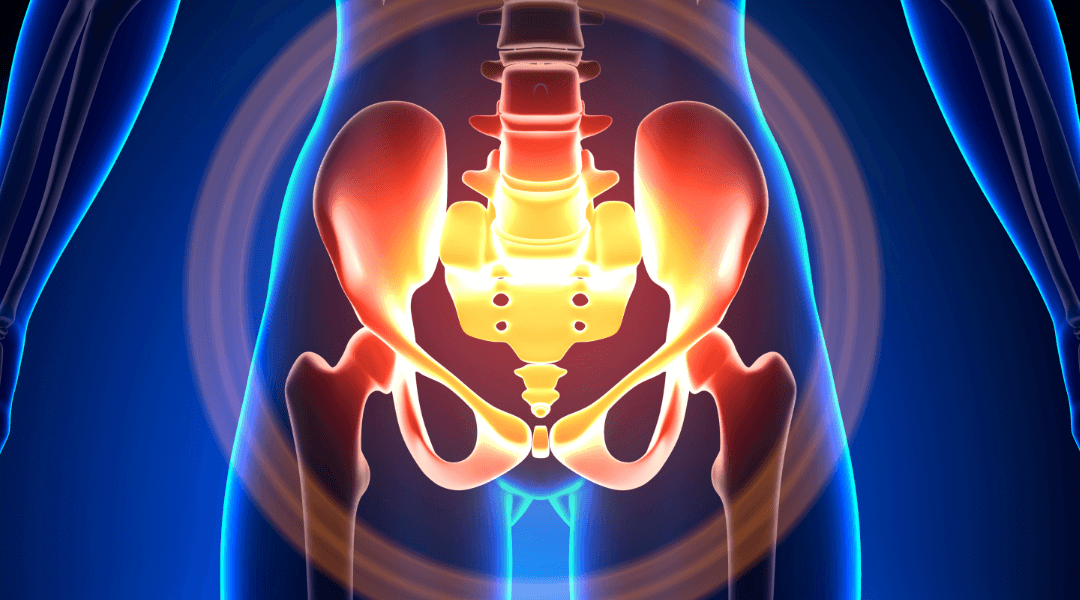
We frequently hear reports from patients that they have been told their SIJ or pelvis is ‘out of place’ or ‘displaced’ causing one leg to be longer than the other and the SIJ being ‘out of place’ puts undue pressure on the lower back or is a cause of their pain. Fortunately, our knowledge of the SIJ has improved through many high quality studies on how the joints move. The gold standard for measuring the movement of the SIJ is via implanting tiny ball bearings in the pelvis and using X-rays to analyse movement. More recently MRI has been used. Below are some scientifically proven facts about the SIJ:
- The SIJs are very stable joints making them hard to injure
- The role of the pelvic joints is to transfer load from the lower body to upper body and vice-versa. The SIJs can safely transfer enormous load safely
- The SIJs have on average 2.5 degrees of rotation (very small) when unloaded and when loaded in standing 0.2 (negligible) degrees of rotation.
- The ability of skilled therapists to clinically detect SIJ movement abnormalities and joint displacement has been compared with MRI, showing the therapist findings have no correlation with the ‘gold standard’ findings
- No study using imaging has detected SIJ positional faults, it’s highly unlikely the pelvis can be ‘out of place’, ‘displaced’ and consequently cause leg length changes
- Additionally, no high quality study using imaging has shown that manipulation can alter the position of the pelvic joints. The reason for the potential benefit of manipulation is complex and any benefit is most likely to be explained by nervous system pain inhibition or improved muscle function following treatment
- Pain from the SIJ is primarily felt in the back of the pelvis and doesn’t refer to the lower back, however, the SIJ can refer pain distally into the leg
- Skilled Physiotherapists can diagnose the SIJ as a source of pain in the clinic using a combination of questioning and tests. Imaging is not routinely recommended
- The pelvic joints are controlled by its ligaments and muscles. Muscles can increase pelvic stability, however, PGP can be associated with too much muscle activity or poor timed and insufficient muscle activity.
- Some of the relationships between pregnancy and PGP has traditionally been explained the increase in relaxin hormone levels during pregnancy. An increase in relaxin levels results in increased ligament laxity, however, multiple studies have consistency found no association between relaxin levels and PCP, disability or pain.

How should PGP be managed?
PGP, the same as other musculoskeletal disorders, should be assessed and managed from a multidimensional and biopsychosocial perspective. This means assessing each individuals unique contributing factors to their pain experience including:
- Movement and muscle function
- Addressing unhelpful thoughts and beliefs around PGP
- Lifestyle factors such as activity levels and sleep
- Clearing any potential contribution from systematic factors such as an inflammatory disorder
With targeted management, most people with PGP will have a good outcome with individualised, contemporary, non-surgical management. At Central Bassendean Physiotherapy we pride ourselves on our accurate diagnosis and evidence based, contemporary management of musculoskeletal disorders. We are happy to have a further discussion on the material presented here or provide the references. You can BOOK HERE or Call us to make an appointment at 9279 7411
Reference
O’Sullivan, P. Beales, D. Diagnosis and classification of pelvic girdle pain disorders-Part 1: A mechanism based approach with a biopsychosocial framework. Manual Therapy (12) 2007
Author

Rob Waller
Senior Musculoskeletal Physiotherapist
Owner
Curtin University WA 2002
Cumberland College of Health Sciences NSW 1988
Rob Waller is a Musculoskeletal Physiotherapist, with over 25 years experience. He is passionate about restoring function following injury and for people with complex musculoskeletal presentations, particularly spinal and shoulder pain. He is also a lecturer at Curtin University teaching on the Postgraduate Clinical Masters program and is currently completing a PhD investigating pain characteristics in young adults using data from the Raine Study Birth Cohort. (http://www.rainestudy.org.au). Other research interests include spinal pain and translation of evidence to practice.