Vertigo
WHAT IS VERTIGO?
Vertigo is a common complaint presenting to both Physiotherapy Clinics and in GP Surgeries. But what exactly is it? What are the most common causes, and how are they managed? Musculoskeletal Physiotherapist Michael Callan will briefly look at the vestibular system, discuss some of the most common causes of vertigo, and outline how Physiotherapy can assist in the management.
Vertigo is not a diagnosis. It is an illusion of motion that is not actually occurring. Common descriptions are spinning, shifting, swaying or rocking. It commonly occurs when something goes awry with the vestibular system, brain, neck, or arteries that supply the brain.
Brief overview of vestibular system
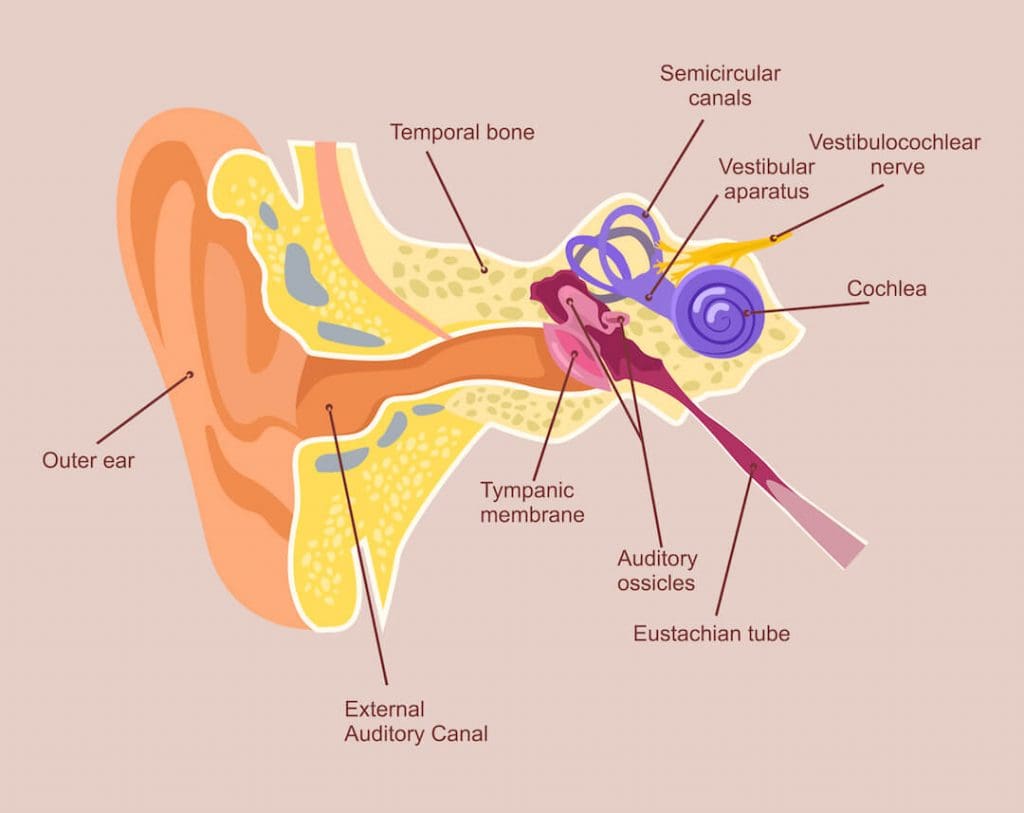
The vestibular system is located in the inner ear, consisting of three semi-circular canals. Its role is to sense head movement and position in relation to gravity. When the head moves, this organ triggers the vestibulocochlear nerve to fire to the brain, telling the brain it is moving. The brain then compares this to information from the vestibular organ in the other ear, the eyes, joints, muscles and ligaments everywhere else in the body, and makes automatic corrections to keep our gaze and balance stabilized.
BPPV – Benign Paroxysmal Positional Vertigo
Benign paroxysmal positional vertigo, better known as BPPV or positional vertigo, is the most common cause of vertigo, making up approximately 66% of cases. BPPV occurs when small calcium crystals break from the inside of the vestibular apparatus and get stuck inside the semicircular canals. As a result, when the head moves, the extra weight of the crystal over stimulates the nerve, telling the brain that the head is spinning when it is not.
Those with BPPV often wake in the morning and experience vertigo and nausea rolling or getting out of bed. Symptoms often ease when the head does not move, but return when the person moves their head.
What causes BPPV is not known for certain. It is strongly associated with age, with those over 50 having a 33% chance of acquiring it. It is also associated with blows to the head.
Treatment of BBPV most commonly consists of the Epley manoeuvre, a technique designed to reposition and remove the crystals from the canals. Repositioning techniques get rid of symptoms immediately in 75% of people, and 85% within three treatments. However, some cases do not resolve immediately, and require additional techniques or vestibular retraining (VRT). Some Physiotherapists and GPs undergo additional training to perform repositioning techniques and VRT, which can be very helpful in resolving an episode BPPV.
Vestibulopathy (Viral Neuritis)
Another common cause of vertigo is when the nerve that travels between the inner ear and the brain is affected, called vestibulopathy. This usually occurs after an inner ear infection or viral infection in the body (viral neuritis), and can be accompanied by signs of immune compromise, like cold sores, fever or shingles. Vestibulopathy can also occur from trauma to the ear, sound abuse, use of certain drugs (‘mycin’ family of antibiotics) or lack of blood flow to the area (diabetes, cardiovascular disease).
Those with vestibulopathy usually report constant vertigo or dizziness, which is worsened by head movement, eye movement and sometimes moving in cars. They often remember a triggering event like an ear infection, where they were very sick and dizzy, or a particular event that caused trauma to the ear like scuba diving where the ear pressure did not equalize. Other symptoms are often present, like ringing in the ears (tinnitus), hearing loss, feeling of fullness in the ear, eye fatigue and headaches behind the eyes, and balance loss.
Management of vestibulopathy depends on where it is during its clinical course. In an acute inner ear infection, medical attention should be sought for appropriate anti-viral and anti-nausea medication. Once the acute phase has passed, vestibular rehabilitation (VRT) is commenced. VRT aims to restore normal function of the vestibular system, balance, eyes, and various reflexes associated with dizziness, and varies from case to case. It can involve balance exercises, eye exercises, and habituation exercises. Habituation exercises involve gradual exposure to motions that cause dizziness in order for the brain and vestibular system to get used to them again. Unlike BPPV treatments that usually lead to symptom resolution in days, VRT is a gradual process that takes many weeks if not months. Physiotherapists with extra training in VRT can educate and guide patients through these exercises, and can provide thorough assessment and information on the process and management.

Cervicogenic
Less commonly, dysfunction of the neck can also cause vertigo. The brain relies on information from the neck to keep the eyes stable when we move, and for information to confirm whether the head is moving or not. Cervicogenic vertigo often occurs after injury to the neck like a motor vehicle accident, or in chronic neck problems.
Management of cervicogenic vertigo depends on the underlying cause of the neck problem. Thorough assessment by a Physiotherapist can reveal what is driving the neck disorder, and appropriate management of the neck often leads to the resolution of both the neck symptoms and vertigo.
Do you have problems with Vertigo? You can BOOK an appointment HERE or Call us at 9279 7411.
Author

Mike Callan
Senior Musculoskeletal Physiotherapist
Curtin University 2010
Throughout his career, Mike has taken every opportunity to learn and upgrade his skills, completing courses in shoulder treatment, neck and back pain, hip and groin pain, gym rehabilitation, dry needling, and chronic pain management. Mike also has experience with sporting injuries as Physiotherapist for various rugby, football and tennis clubs around Perth, as well as being part of medical teams for various tri-sport events in WA.