What is Frozen Shoulder?
FROZEN SHOULDER
Frozen shoulder typically involves substantial pain and a significant reduction in ROM at the glenohumeral joint of the shoulder complex. Historically this has been difficult to treat, and mistruths persist today that stem from early clinical observations. However, a clear evidence-based pathway has developed in recent years to manage frozen shoulder with good outcomes.
So, what do we really know about Frozen shoulder? Frozen shoulder can occur of its own accord or secondary to trauma (such as post surgically or after an injury). In Japan and China frozen shoulder is known as the ‘50 year old shoulder’, as this reflects the average age of the presentation. It does not affect women more than men. People with diabetes, thyroid abnormalities or heart disease display a higher incidence of frozen shoulder. The pathology involves a substantial thickening of the shoulder capsule and ligament. It does not involve adhesions of the capsule to the bone (head of humerus), thus shouldn’t be called adhesive capsulitis.
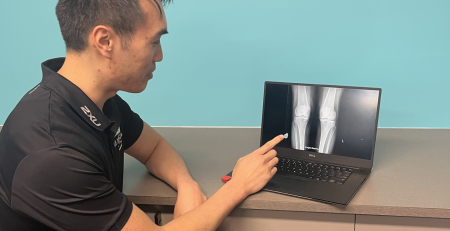
There is no ‘gold standard’ of how to identify frozen shoulder and arriving at a diagnosis may take some time due to a variety of conditions that may present with increasing pain. The simplest clinical criteria involves an equal restriction of the active and passive glenohumeral range of motion with a normal shoulder x-ray. An X-ray maybe required to exclude presentations such as osteoarthritis, sarcoma, dislocation, avascular necrosis that may also painfully restrict movement. Frozen shoulder has typically been classified into multiple stages, however this can be simplified into two phases to better guide management. The initial phase is pain > stiffness, the latter stage stiffness > pain.
The name frozen shoulder implies that the shoulder will eventually ‘thaw’, but does frozen shoulder resolve on its own? Despite most patients being told that the average duration is 30 months, more recent studies have indicated that up to half the patients with frozen shoulder still experience some pain +/- stiffness at 7 years following diagnosis (Schaffer 1992). The ‘’wait and see’’ approach has no evidence to support the theory of recovery to full resolution without treatment (Wong 2017).
A more proactive approach to managing frozen shoulder yields good results, but first a definitive diagnosis is required. Jeremy Lewis, a leading shoulder research expert has developed a pathway of care for the initial stage of frozen shoulder that involves:
- Corticosteroid injection of the shoulder joint.
- Gentle self-assisted shoulder movements for one week following injection.
- Physiotherapy for joint mobilisations, soft tissue release, home exercise prescription and passive movements from one week to four weeks post injection.
- If pain is not decreasing as expected after four weeks, consider reinjecting providing there is at least one month between injections and there have not been more than 3 injections in one year.
Ultrasound guided cortisone injections (combined bursa and glenohumeral joint) have strong evidence for pain reduction in the short to mid-term with limited effect on the shoulder range. These injections have the best outcome when combined with physiotherapy, as this enables a faster transition through the pain > stiffness phase.
Continuing use of the shoulder is recommended with recent evidence (Rawat 2017) showing a significant role for specific strengthening exercises (when compared to manual therapy alone). This proactive approach of physiotherapy management of frozen shoulder yields improved function, reduced pain and increase range of movement in the short term.
If you would like to talk about whether physiotherapy is appropriate for you, don’t hesitate to call and chat.
Simply BOOK an initial consultation HERE with a Physiotherapist or call us on 9279 7411.
References;
Schaffer et al (1992) Frozen Shoulder – a long term follow-up Journal of Bone and Joint Surgery-Am vol 74:738-746
Wong et al (2017) Natural history of frozen shoulder- fact or fiction? Physiotherapy 103:40-47
Lewis (2015) Frozen shoulder contracture syndrome – Aetiology, diagnosis and management. Manual Therapy 20:2-9
Rawat et al (2017) Frozen Shoulder: Is there a role for strengthening exercises? Journal of Hand Therapy 30:235-241
Author

Lindsay Alsop
Senior Physiotherapist
Curtin University 2009
Lindsay is a musculoskeletal physiotherapist who has worked in private practice since graduating. He prioritises functional outcomes for the patient when returning them from injury and strongly advocates physical activity to maintain a quality of life. Read more here …