What care should you receive when you have musculoskeletal pain?
Here are 11 recommendations for high quality care.
I was recently heavily involved in research team that identified 11 common recommendations for musculoskeletal pain care 1 . To do this, we summarised the results of recent high quality clinical practice guidelines for a variety of musculoskeletal pain conditions (low back, neck, knee, osteoarthritis, and shoulder). We identified common recommendations across all guidelines. To highlight how might these guidelines be relevant for the average person, there is a brief example below.
You spontaneously developed low back over 2 months ago and it still hasn’t settled down. You don’t remember doing anything in particular, but you’ve been working longer hours lately! Maybe you should go and see your GP and ask for a scan? Or maybe see a physio? Your brother-in-law saw a specialist for “injections” many years ago. Perhaps you should too?
This example highlights thoughts that can go through your mind when you have an episode of musculoskeletal pain. Musculoskeletal pain complaints, such as back and neck pain, knee pain, osteoarthritis, and shoulder pain, are very common, affecting about 1 in 3 Australians 2 . There are a range of scans, treatments, therapies and surgeries that are available, enough to confuse the most well informed person! These interventions can be expensive and often have poor outcomes 3 .
What should you do? If you see a practitioner for help, how do you know that you will be receiving the right care at the right time?
These recommendations summarise current ‘best-practice’ and can act as a guide for you to use if you attend a health care appointment with a musculoskeletal pain complaint. They apply to the care you might receive from health practitioners of any profession. They can also be used by health practitioners to assess whether what they are doing is of high value and reflects ‘best-practice’.
The 11 recommendations are:
1. Care should be patient centred.
This means that care should respond to your situation including your preferences and values. You and the health practitioner should use a shared decision-making process to come up with a management plan together.
2. Practitioners should screen patients to identify those with a high likelihood of serious pathology/red flag conditions.
‘Serious pathology/red flag conditions’ are conditions that present like a musculoskeletal pain condition but that require medical care (e.g. infections, cancers, rheumatoid arthritis). Screening involves appropriate thorough questioning and a clinical examination.
3. You should not be referred for radiological imaging unless: (1) serious pathology is suspected, (2) there has been an unsatisfactory response to conservative care or unexplained progression of signs and symptoms or (3) imaging is likely to change management.
Radiological imaging such as x-rays, CT and MRI scans are helpful, such as if a ‘red flag’ is suspected. However serious pathology such as cancer, infection, or fractures occur in less than 1% of presentations 4 . Imaging is not routinely required for musculoskeletal pain and a large percentage done is deemed inappropriate 3 . Receiving an x-ray or scan when it is not warranted results in worse outcomes for patients, especially as it increases worry, results in unnecessary radiation exposure, and can escalate health care that is not needed, including surgery 5 .
4. Psychosocial factors should be assessed.
Psychosocial factors are your emotions, beliefs and expectations, as well as your social circumstances, such as your work and home situation and social support structures. These factors can have a powerful influence on how susceptible you are to having a flare up of pain in the first place, and how well you recover 6 .
5. You should receive a physical examination.
Examples of a physical examination include tests to assess your movement, muscle function, and tests of your nervous system.
6. Your progress should be evaluated.
For example this could be assessed using questionnaires or measures of your function (what you can do/not do), your recovery, pain intensity and quality of life.
7. You should be provided with education/information about your condition and management options.
This is to inform and reassure you about your pain, discuss relevant psychosocial aspects such as unhelpful beliefs and to assist you to self-manage e.g. through exercise.
8. You should receive management that addresses physical activity and/or exercise.
Movement and exercise keep the musculoskeletal system and body healthy. Exercise is the best medicine that money can’t buy! When you have musculoskeletal pain it is usually helpful to increase general (e.g. walking) or specific exercises (e.g. muscle strengthening) to manage your condition. Occasionally you may need to modify what you are doing or do less to avoid
aggravating pain.
9. If used, manual therapy should be applied only in conjunction with other treatments
Manual therapy includes hands-on treatments such as massage, manipulation and mobilisation. If your management includes manual therapy it should be part of a management package that also includes exercise and information/education, and potentially psychological therapy.
10. Surgery should only be considered if non-surgical care has been ineffective.
Except in special circumstances (e.g. a ‘red flag’ condition), non-surgical care such as exercise and rehabilitation should be used as first line measures. A poor outcome from non-surgical care does not necessarily mean surgery becomes a good option.
11. Keep working or resume work as quickly as possible.
If you work in a satisfying workplace, then staying at work or getting back to work as quickly as possible, helps recovery from musculoskeletal pain. To do this, modified duties may be needed.
This list of recommendations for high-quality care may evolve as further research is undertaken. For example we know that having a generally healthy lifestyle is beneficial for musculoskeletal pain, such as avoiding smoking, sleeping well and maintaining a healthy weight, but this has not filtered through into clinical practice guidelines as yet.
But for now, if you do experience an episode of musculoskeletal pain and seek care, these recommendations can be a guide to make sure you are receiving the best quality care! Better still, if you are being affected by musculoskeletal pain, our Physiotherapists at Central Bassendean Physiotherapy are passionate about providing ‘high value’ care to keep you doing the things that are important to you.
Conveniently located in Bassendean, our clinic is within close reach from surrounding suburbs Morley, Eden Hill, Caversham, Bayswater, Guildford, Ashfield, Ascot and South Guildford.
To book an appointment, please call us today on (08) 9279 7411. We can help you!
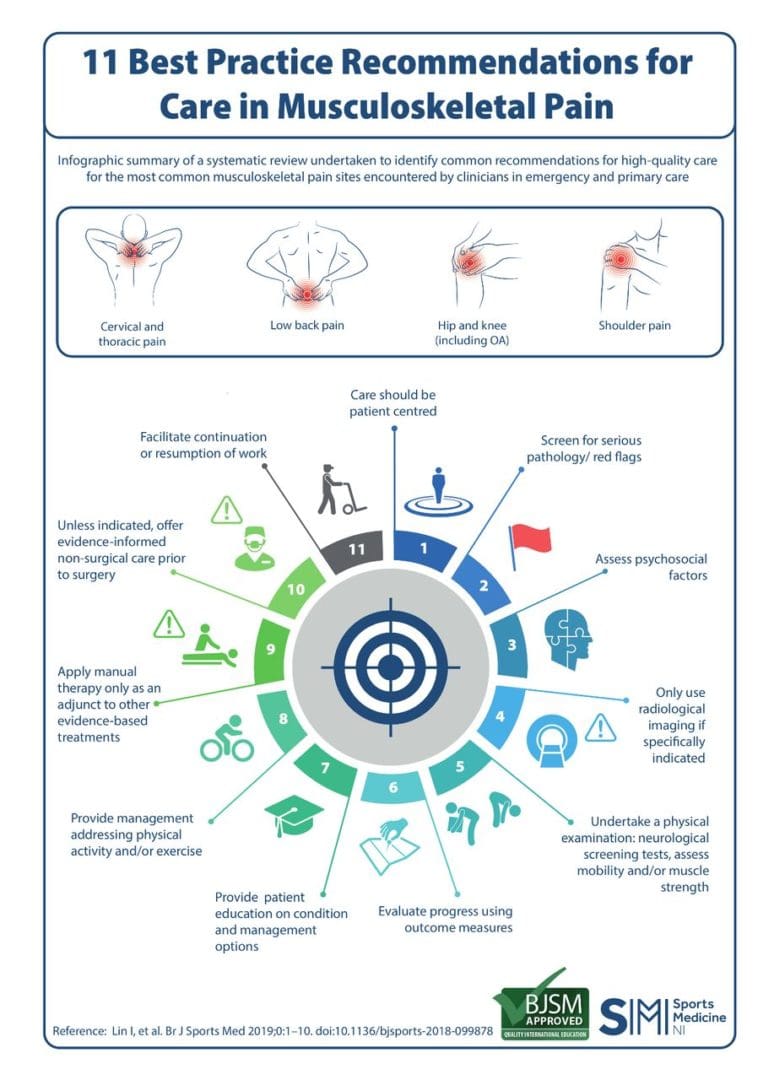
An infographic of the 11 recommendations for musculoskeletal pain care 7
References
1. Lin I, Wiles L, Waller R, et al. What does best practice care for musculoskeletal pain look like? Eleven consistent recommendations from high-quality clinical practice guidelines: systematic review. Br J Sports Med. 2019:bjsports-2018-099878.
2. Australian Institute of Health and Welfare (AIHW). The burden of musculoskeletal conditions in Australia: A detailed analysis of the Australian Burden of Disease Study 2011. Canberra: Australian Institute of Health and Welfare;2017.
3. Lewis J, O’Sullivan P. Is it time to reframe how we care for people with non-traumatic musculoskeletal pain? Br J Sports Med. 2018.
4. Henschke N, Maher CG, Refshauge KM, et al. Prevalence of and screening for serious spinal pathology in patients presenting to primary care settings with acute low back pain. Arthritis Rheum. 2009;60(10):3072-3080.
5. Darlow B, Forster BB, Sullivan K, Sullivan P. It is time to stop causing harm with inappropriate imaging for low back pain. Br J Sports Med. 2016.
6. Pinheiro MB, Ferreira ML, Refshauge K, et al. Symptoms of depression as a prognostic factor for low back pain: a systematic review. The Spine Journal. 2016;16(1):105-116.
7. Lin I, Rankin A, Wiles L, et al. Infographic. 11 best practice recommendations for care in musculoskeletal pain. Br J Sports Med. 2019:bjsports-2019-100821.
Author

Rob Waller
Senior Musculoskeletal Physiotherapist
Owner
Curtin University WA 2002
Cumberland College of Health Sciences NSW 1988
This month’s blog post is by our Owner, and Senior Musculoskeletal Physiotherapist Rob Waller.
Rob Waller is a Musculoskeletal Physiotherapist, with over 25 years experience. He is passionate about restoring function following injury and for people with complex musculoskeletal presentations, particularly spinal and shoulder pain. He is also a lecturer at Curtin University teaching on the Postgraduate Clinical Masters program and is currently completing a PhD investigating pain characteristics in young adults using data from the Raine Study Birth Cohort. (http://www.rainestudy.org.au). Other research interests include spinal pain and translation of evidence to practice.
To view all of Rob’s publications, click here: View Publications